
To ease the administrative burden and increase efficiency of case management calls, enGen partnered with Laguna Health to provide AI assistance for a large payer client’s case management team.
Case managers get satisfaction from supporting members so they can improve their health. On member calls, clinicians strive to develop a meaningful dialogue so they can determine health challenges and get members the care they need. While documentation and other administrative tasks are necessary, they often compete for the case manager’s attention during calls.
With support from enGen and Laguna Health, case managers are spending less time documenting calls and more time identifying personalized action items to improve member care.
Points of Success
66%
cut in call documentation time
27%
increase in clinician satisfaction with call prep efficiency
94%
of call summaries needed only minimal clinical edits
+96
annual enrollments possible per case manager
Industry Challenge
For case managers, taking notes during and after member calls can feel burdensome at times. They must document their calls to effectively coordinate the care plan and comply with regulations. Yet optimal interactions involve listening to a member’s needs, expressing empathy and understanding, and finding solutions on the spot that support the member’s health.
When a case manager winds up spending more time preparing for calls and summarizing conversations than talking with members, both sides of the equation suffer. Members aren’t happy if they have to wait for a case manager to become available. And case managers are more likely to experience burnout if they don’t feel they’re providing enough personalized attention to members’ care needs.
Payers want their clinicians to provide top-notch attention to their members. Addressing medical needs early can avoid more expensive and complex treatment down the road. And clinician-member interactions affect the quality of care and member satisfaction ratings.
Solution from enGen to Laguna
To arm our large Blue Cross Blue Shield insurance client with tools to optimize case management calls, enGen teamed up with Laguna Health. Laguna specializes in conversational AI designed for care teams within health plans and virtual care organizations.
We collaborated with Laguna to bring conversational AI capabilities into the client’s case management solution quickly and with little disruption or change management. The partnership has enabled Laguna’s AI tool to listen in the background, provide helpful prompts to case managers, and speed call preparation and documentation.
With these new capabilities, our payer client has gained automated support for member calls. The Laguna Companion helps with these aspects of a case manager’s work:
• Records member calls to provide real-time insights, transcripts, and post-call documentation.
• Prompts the case manager with questions to ask the member, based on the content of the conversation.
• Suggests actions the case manager could take to support the member.
• Provides feedback to the case manager on ways to improve phrasing and interactions with members.
• Provides indications that a case manager is getting fatigued.
• Creates time-saving call summaries, tailored to each team’s specific requirements, and syncs with Predictal’s Case Management module.
The workflows always keep humans at the helm. enGen and our client only automate with AI when no adverse determination would affect members or providers.
Clinicians review and edit the automated summaries. Their managers monitor dashboards and track clinician accuracy, efficiency, effectiveness, burnout risk, and quality outcomes.
Successful Proof of Concept
Before going live with AI assistance for all the client’s case management teams, Laguna and enGen conducted a 90-day pilot with 31 clinicians. We collaborated to deploy the AI tool to support member calls. Features include listening and providing insights, giving live clinician feedback, automating documentation, and enabling data sharing, analysis, and reporting.
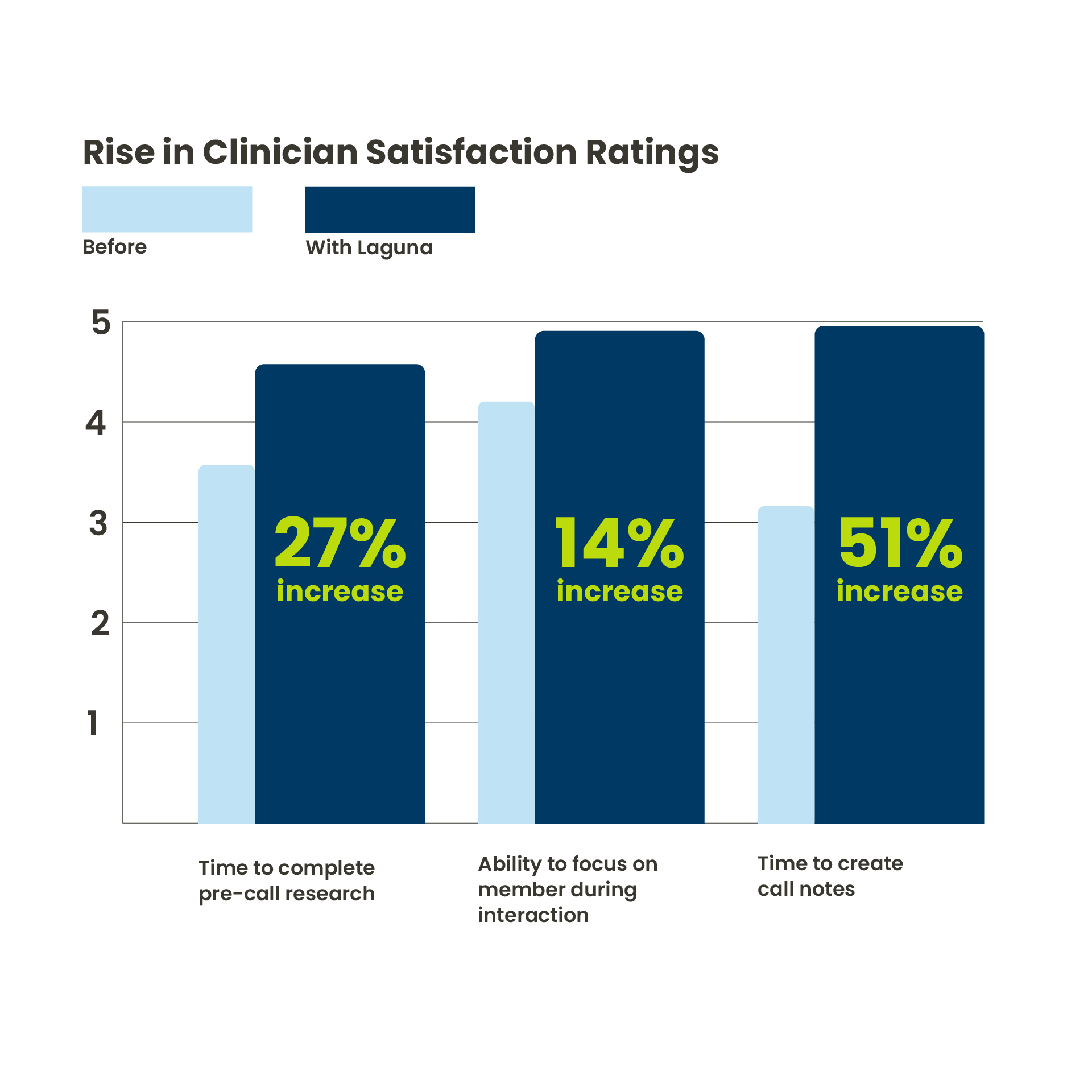
Our client surveyed their case managers before and after the pilot, comparing clinician impressions of member calls with and without AI assistance. The proof of concept revealed favorable experiences from case managers using the AI tool in their workflows.
One pilot user said, “My confidence and quality of calls has improved so much.”
Another shared, “This is going to help us be quicker and make us better nurses.”
These outcomes underscore the real-world impact of the pilot – streamlining workflows, improving clinician satisfaction, and enabling more personalized member care. Highlights from the pilot include:
•Automated note taking freed up time for a closer focus on member concerns.
•Automated workflows sped up documentation and increased efficiency.
•AI assistance captured emotional tone and prompted case managers with empathetic follow-ups.
•Feedback provided strategies for case managers to improve their approach.
•Call summaries demonstrated high accuracy and captured emotional nuances.
•Automated support for administrative tasks eased case manager stress.
With personalized feedback for member conversations and suggestions for case managers’ professional growth, users reported improved performance and quality outcomes.
“At enGen, we’re committed to providing tools to advance payer operations and boost satisfaction. Our partnership with Laguna is yielding wins for busy case managers and their members,” said Stimpson.
AI Yields Empathetic Messaging
The word “empathy” came up in several aspects of pilot user survey results.
Case managers liked how the AI assistant infused empathy into suggested questions during calls. The tool identified members’ emotions and prompted the case manager to respond supportively.
That aligns with a university study that found AI-generated messages supported recipients in feeling heard better than untrained human responses.
In the Laguna pilot, case managers also liked the empathetic tone of professional development recommendations. During and after calls, the AI tool provided suggestions for improving clinicians’ effectiveness.
The combination of more time for focused human attention, automated note taking, personalized AI prompts, and opportunities for professional growth made a positive impression on pilot users.
Expanding the Approach
Because the feedback from clinicians in the pilot has been so positive, other teams have expressed interest in using Laguna. Based on that initial success, the client gradually scaled access to more than 300 case managers using Laguna Companion by May 2025.
enGen facilitated the expansion by making it easy for the client to add Laguna functionality for telephony system users. Once all case managers are on board, the API interface to Predictal will enable call notes to automatically flow from case managers into our Case Management module, saving even more time.
“We’re facilitating smooth data exchange to minimize manual processes and propel the benefits of AI and automation even further for our payer client,” said Stimpson.
Client managers applauded how well the partners worked together with open and honest communication, mutual respect and trust, and responsive support and updates during the pilot. They are excited about bringing this technology and its advantages to more of their clinicians.
Using healthtech tools from Laguna and enGen, our client is advancing clinician efficiency, competency, and satisfaction for a job well done.
How Can enGen Help You?
Achieving optimal health outcomes demands seamless alignment of people, processes, and technology. By uniting human decision-making, AI technology, intelligent automation, and healthcare operations knowledge, enGen drives strategic innovation as a partner for payers.
Our AI program focuses on human-led ethical solutions, ensuring peace of mind for payers, providers, and members. More than a technology partner, enGen is committed to building a future where technology empowers human expertise to support healthier lives for all.
Let us help you find healthtech solutions to reach your team’s evolving goals.


